The two big topics of this week – emergency pressures and raising concerns by staff – are very closely linked

Pressures on hospital A&E departments
We have experienced extreme A&E pressure since the Bank Holiday. While attendances remain high, at Heartlands Hospital we have seen discharges fall, and a dozen fewer patients discharged each day over the period mean that we have the equivalent of an additional ward of inpatients
This means the length of time for a bed to become available increases, and pressure builds up in the Emergency Department. As most local hospitals have been in the same position we are unable to divert ambulances to gain some respite. Our clinical teams have worked tirelessly to manage the situation, which will only ease as we increase our discharge rate and free up capacity to allow ‘flow’ to resume
Why has this happened? High attendances are a factor, and we need to make sure that we keep our Emergency Departments for those that really need them. There remains an urgent need for responsive alternative services, with sufficient capacity so that our hospitals are able to focus on what they are designed to do. The discharge side of the equation is critical though, and while the numbers do fluctuate the holiday period is certainly a factor. Both within hospital, and outside in community and social care services, our services are people based so key people being on leave does impact on performance, particularly when margins are tight and headroom is minimal, as they tend to be in our system
This pressure impacts on our staff as well as our patients, of course, and as we encourage staff to raise concerns it is no surprise that the emergency pressures are reflected in the feedback we receive?
Raising concerns
We have been thinking about how we can make it easier for staff to speak up. At our weekly new staff induction I always include this topic in my welcome, explaining both the importance of speaking up and the ways to do this
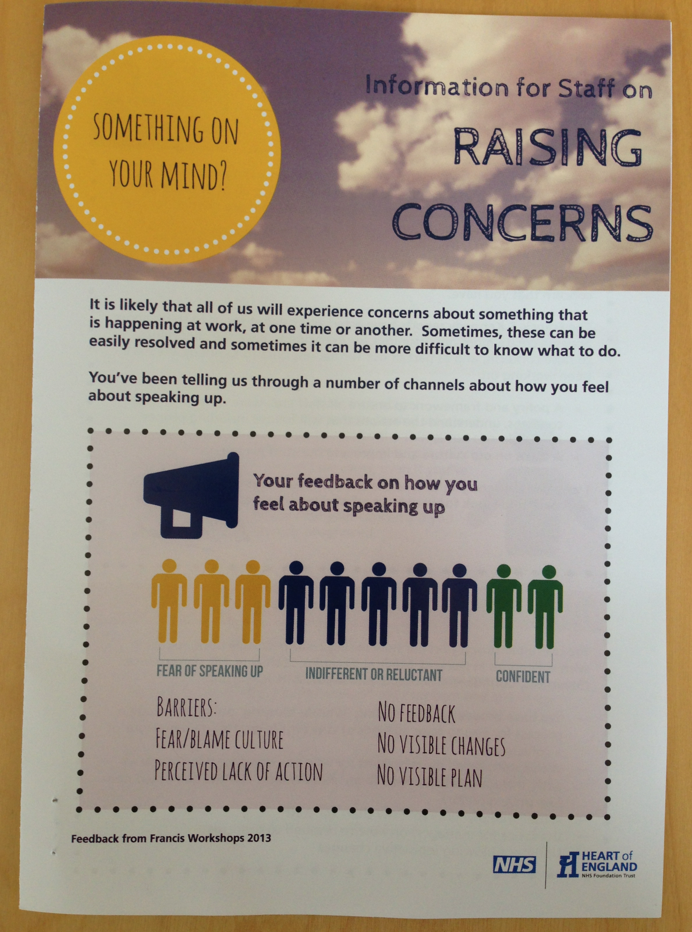
We have revised our policy in light of the Kennedy Review, and an explanatory leaflet went out along with a message from me with pay slips this week. It is important that we keep talking about this because the first of our internal staff surveys (more on this in future blogs) tells us that staff do still fear the consequences of speaking up. Only 20% felt completely confident to do this, and half expressed either indifference or reluctance
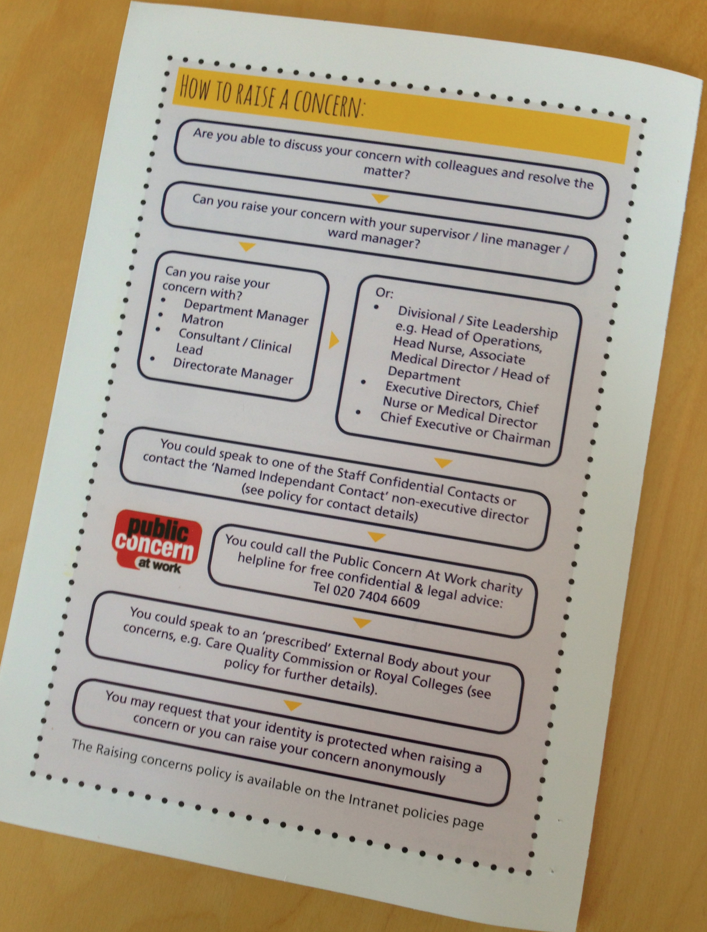
Within 24hrs of the leaflet going out, three members of staff raised with me directly their concerns about the impact of overcrowded emergency areas on patient care. This is pleasing because it shows our approach does lead to staff coming forward who may not have done otherwise, even if it is a risk we are well aware of and one we have been tackling as our top priority for many months now
Our recent reorganisation puts our operational challenges at the centre of all we do. On top of this, I must keep it at the top of the agenda for the wider health system, because hospitals are only one part of a complex system of care provision. If the system struggles, either with alternative services to hospital, or with accepting discharges from hospital, then it tends to be our A&E departments where the pressure is felt most acutely
I have written many times about this matter. Our staff are telling us clearly that it remains a challenge, despite the best efforts of many. More to do, and a topic that will feature often in the discussions of our new Staff Engagement Group I’m sure!
Car parking
This thorny issue cropped up without warning in the national media last weekend! I know from discussions I have locally that it remains a contentious subject for many people
It will always cost money to provide hospital parking, for staff, patients or visitors. Managing car parks so that space is available to those who need it, when they need it, requires barriers and staffing. Without these, our car parks would be full of workers, shoppers and others and continually full. And as demand grows, investment is needed in additional space too
Rightly or wrongly, we have evolved a system whereby this funding comes from those who use the facilities. Car parking is funded by those who park, so any change will inevitably mean that resource has to be diverted from elsewhere. Those who come by public transport, or who are brought by others, will oppose this – I know this to be true because many have told me!
Of course, none of this justifies the imposition of unreasonable charges, or poor management that results in frustration and delay for people who are understandably anxious about coming to a hospital
We recently introduced a much reduced fee for those needing to park regularly. I was challenged as to why only cancer patients got free parking, when people with many other conditions also needed to make repeated visits – a fair point. So we have introduced a 20 visit ticket that costs £10, meaning that parking costs 50p however long the stay. It is available on the signature of the relevant Ward Manager and is not confined to those with specific illnesses
We are also making it easier for those who are exempt from charges to claim them back – many people are eligible for this but not aware
Finally, we are investing the revenue we receive in additional car parking capacity, and this shouldn’t be overlooked. We recently built a new multi-storey car park at Heartlands, creating extra spaces for staff and visitors. Another is planned for Good Hope Hospital
We will look closely at the new guidance – although we believe we are largely compliant there is always room for improvement. Of course, as with emergency pressures, hospitals are part of wider communities, and better provision of alternative means of travel would be a much better solution to this perennial challenge!
Do visit our weekly Health Blog Round Up
Mark Patel
Hi Mark
Car Parking, what a nightmare topic, it seems whatever the NHS does, someone somewhere will criticise.
In my opinion, Mr Hunt’s comments last week were unhelpful at best. Exactly as you say, car parks cost money to run and maintain, and simply being told to provide free parking means that already cash-strapped hospitals must divert money from nurses & doctors wages and medicine to pay for the car parks.
Where “we” (the NHS) would benefit is being certain our car parks are self-funding, and not being run at profit, and do everything possible to not penalise those that are suffering the indignity of chronic diseases that require multiple hospital appointments.
Which may include discounted or free rates, making damn sure that we do what we said when we said (appointment times), etc.
and there’s my two pennies.